Welcome to Dr. Nelson's
Fingertip Amputations
First posted April 9, 2008 Last updated October 28, 2014
![]()
|
You are here because you have cut off part of your fingertip (the last joint of the finger is still present). (This page does not cover finger amputations and replantations, or fingertip crush injuries, which are entirely different topics. Read on to see if this is the right page for you and if not, where to go.) (see also Fractures and Fingernail Fungus Infections; surgeons, note a link at the bottom of the page for further information.) |
![]()
Is This the Right Page for You?
First of all, you need to determine if this is the right page for you. This page covers fingerTIP amputations, not finger amputations and not fingertip crush injuries. The reason for the different pages is that they are treated in dramatically different ways.
DEFINITIONS
Fingertip amputations: part of your fingertip was cut off, but the last joint of your finger (the one next to the nail) is still there. This is the right page for you, keep reading. To start with, you can get a good idea of how great these injuries usually heal by looking at this video of the healing of the fingertip amputation of a surgeon.
Fingertip crush injuries: your fingertip was crushed, not cut, and essentially all the parts are still there, just mushed. This is NOT the right page for you, read Fingertip Crush Injuries here on my website.
Finger amputation: all or part of your finger (or hand or arm) was cut off, including the joint next to the tip of your finger. I do not have a page on this topic. These injuries may be considered for replantation with microsurgery.
Fingertip Anatomy
The fingertip is a highly specialized structure, with many specialized features. It has a lot of nerves, as I am sure you are more aware of than you would like! The illustration below shows many of the important structures of the fingertip. This image is from the book, The Fingertip, by Dr. Zook.
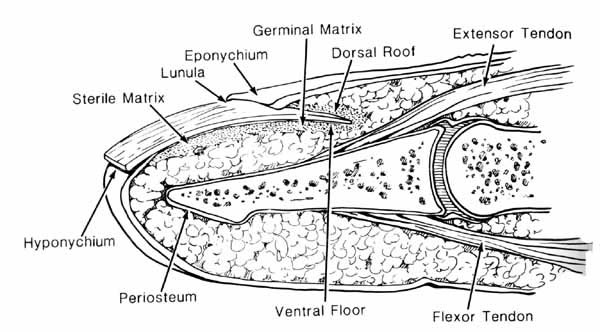
The fingernail itself, the thing that you cut with a fingernail clipper, is called the nail plate. Underneath the nail plate is the nail bed, the mostly pink tissue you can see under the nail. It has several regions. The proximal (this is a medical term that is good to understand, it means that part closer to the heart; the opposite direction is called distal) part of the nail plate is called the germinal matrix. This is the part of the nail bed that originates the nail plate. When you look at your fingertip, part of the germinal matrix can be seen through the nail plate: it is the white moon-shaped area. The name for this is the lunula. That is, the lunula is the visible part of the germinal matrix. The majority of the germinal matrix is not visible, and it is located under the proximal nail fold, or eponychium. The cells of the dorsal roof in the eponychium are responsible for placing the shine on your nail plate. The hyponychium is a specialized structure uner the nail plate at the distal end. Its purpose is to help prevent dirt and bacteria from entering under the nail into the nail bed. It is backed by specialized capillaries (small arteries) and lymphatics that also help to prevent the invasion of bacteria or funger under the nail plate. The fingertip is also an organ of temperature regulation: if you are hot, special valves open up to allow increase bloodflow to your fingertips. If you are cold, these valves shut off (this explains why your fingertips get so cold in cold weather!) The fingertip is a very specialized structure!
Fingertip Amputation Injuries
There are many levels or kinds of fingertipamputations, as shown in the diagram below. This classification is called the Allen Classification, and is used for sharp amputations that are fairly straight across the finger. The classification breaks down when the cut is very oblique, for instance, removing all of the fingertip pad but none of the nailbed.
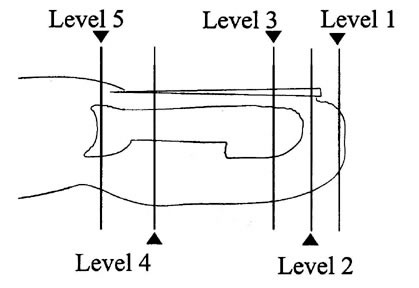
The Allen Fingertip Amputation Classification
Level 1 involved only skin. Level II involves both skin and bone. Level III involves some loss of nailbed. Level IV involves the germinal matrix and often some of the nail fold. Level V involves the insertion of the tendon. Each amputation level has unique implications for treatment and outcome.
There are many other considerations besides just the level of the amputation. The nail bed can bleed, which creates a collection of blood
(called a hematoma) under the nail plate. This is called a
subungual hematoma. They can be very painful, and need to
be drained. This usually dramatically decreases the pain of a fingertip
injury. Fractures of the fingertip, usually of the type called a tuft
fracture, usually heal well if given a chance to rest. A splint
and rest is all that is needed.
How Are Fingertip Amputation Injuries Treated?
This is a great question, but the variety of injuries is so broad that it is hard to give you a specific answer. In general, fingertip amputations can be closed by taking part of the fingertip that was amputated, removing the bone and fat, and placing it back on the fingertip as a full-thickness skin graft. Most often, when the amputated part is not available to act as a skin donor, the would will be cleaned and covered with a special dressing called Tegaderm, which is a semipermeable membrane. This allows new skin to grow, nurtured by the healing fluids that accumulate under the dressing. Sometimes the open area is closed by moving some of the adjacent skin to close the wound. This is done particularly when there is a very large open wound and the amputated fingertip is not available. Each situation has unique characteristics, but this will give you an idea of the various options available to treat your injury.
What Kind of Results Can I Expect?
Almost all fingertip amputations start out looking horrible, and almost all of them result in a finger tip that is not normal, but is so highly functional that the patient has no disablity at all. Here are two examples. The first is of an Allen III (skin, nail bed, and bone), a fairly significant injury) that was very oblique (more tissue was lost from one side than the other), which is harder to treat than the straight-across injuries:

This is Dave's finger when we started. The wound extends all across the fingertip, right to left and top to bottom.

The fingertip has been cleaned and is ready for the skin graft. Note that more tissue is missing from one side than the other but the injury goes all the way from one side of the finger to the other. There is bone exposed in the center of the wound and the nail plate has been removed.

The skin graft has been sewn onto the fingertip.

Here is the fingertip at 5 weeks. Note that the old fingernail is beginning to fall off
and the skin graft is black,
is starting to fall off, and looks dead. It is not!
Note also that the contracting wound has pulled in normal skin from the far side of the finger.

Here is Dave 9 weeks after his injury. Notice that it is hard to tell which fingertip he cut off!

This is the palm-side view. Notice how rounded out the fingertip is.
It is not normal, but it does not hurt, Dave is back at work as a tree trimmer, and the fingertip works great.
Most fingertip amputations at this level do this well.
![]()
This patient is a young woman who cut off the tip of her finger accidentally with a pair of scissors. She was worried that her hand would be deformed for life. Not so! Read on.

Here she is on the day of injury. Note that the tip of the index finger is cut off quite straight
and that there is missing skin and nail bed.
There is no missing bone.
The tip could not be found,
so the wound was covered with a special dressing called Tegaderm and changed at 5 days.

The wound was checked at 10 days, with some sign of healing.
The Tegaderm dressing was replaced.

This is the wound at 20 days. Note that there is some very wet-looking tissue forming on the tip.
The wound was covered with a non-adherent dressing, but not Tegaderm.

This is the wound at 34 days. The normal skin tissue has been pulled into the wound by the healing tissue.
It is not longer wet, but looks like young skin!

These last two pictures are at 48 days. Note that the fingertip has a much more rounded, although not normal, contour.
Almost no one will notice this slightly rounded contour.

This is a side view. Compare it to the first photo: the index tip is now rounded, with normal-appearing skin.
No further care was needed.
Note for Surgeons |
![]()
I hope that this information helps you understand and take care of your fingertip amputation, and supplements the explanation I gave you in the emergency room or the office.
![]()
|
Would you like to search the medical library of
the National Library Medicine for scientific papers on this topic?
Just click on
|
Remember the admonition from the Patient Education Links Page: the Internet has a lot of information, much of it incorrect. I have reviewed the sites that I have linked to, and have only linked to sites when I personally know the surgeon who posted it, or am a member of the organization that posted it. However, I may not agree with all that is on that site, and it may have changed since I reviewed it. If any of the information is not consistent with what I have told you, please download the material and bring it in.
